Healthcare equity marketing plays a crucial role in addressing health disparities in the United States. Many people live in areas without proper access to medical care, while some cannot afford to see a doctor.
The challenges to addressing health disparities are ample, and attaining health equality is not easy.
But to overcome the startling healthcare problems, it is imperative to understand the whys and hows of health equity.
Read on to discover the most common health disparities that are gatekeeping equitable healthcare for all.
What is Health Equity?

Health Equity is when every individual gets an equal chance to be healthy. It means ensuring that individuals with health problems, such as diabetes, have access to quality healthcare, regardless of health disparities.
In simple words, it means the opportunity to live a healthy life, whether
- You are rich or poor,
- Male, female or other
- Live in the city or the countryside,
- Follow a different culture, or
- Speak a different language
However, according to the recent release of the Organisation for Economic Co-operation and Development’s (OECD) 2023 Health Statistics, America’s health outcomes are no better than those of other developed countries despite higher healthcare spending.
Thus, America needs policies, communities, organizations, healthcare systems, public health policymakers and agencies to work together and design a system based on health equity.
Why is Health Equity a Must?
Imagine not getting treatment because you are an immigrant! Or imagine a healthcare professional not giving you medication because you belong to a different religion.
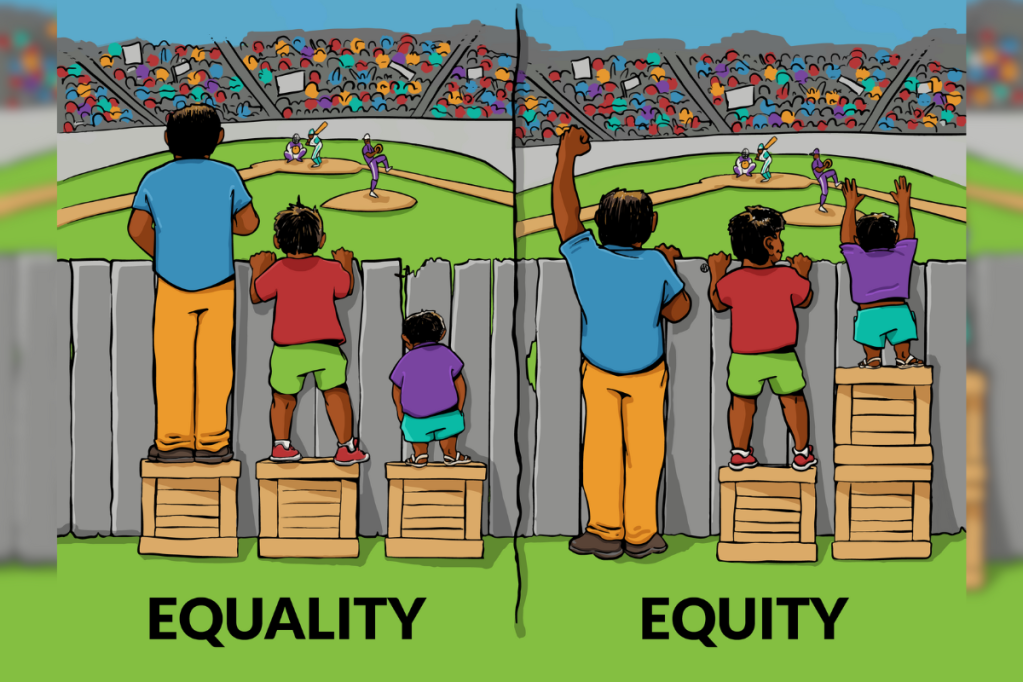
The concept of health equity in the United States is similar to how artist Angus Maguire explains his cartoon. Everyone wants to and can watch the match, but not everyone has equal access to it.
Is it fair? No!
Likewise, medical treatment shouldn’t be denied because you cannot speak a specific language or belong to a rural area. Every individual deserves a fair and equal right to be healthy, no matter who they are or where they come from.
Thus, it is crucial to overlook the health disparities and level the playing field to attain health equity.
How Significant is Health Equity in the United States?
Theoretically, everyone in the United States has access to health care. But if you scratch beneath the surface, the picture is quite alarming.
Let’s see some statistics that will prompt you to push the ‘re-think’ button:
- Report by Steven H. Woolf: The health of US citizens is declining relative to other high-income countries, leading to significant health disparities.
- A Survey by the National LGBTQ Task Force: According to the survey, 50% of trans respondents said that they had to teach their doctors about trans healthcare.
- A report on Mental Health Disparities by the American Psychiatric Association: The report mentions that LGBTQ people are 2.5 times more likely to experience substance abuse, anxiety and depression than heterosexual individuals.
- Data by the National Institute of Mental Health: Approximately 57.8 million adults have some mental ailments. The majority of mental illnesses go untreated, particularly in communities of color, even though the rate of mental health disorders among whites is comparable to that of persons of color.
- A Report by Statista: The report shows how social demographics still impact people’s health in the US.
Health equity for Americans is crucial to overcoming these and other similar discrepancies. But breaking the barriers to health equity is also a mountain to climb to achieve equal optimal health.
Let’s have a look at the obstacles that are curbing unbiased healthcare for all.
Breaking 6 Key Barriers to Health Equity in the US

The prognosis and opportunities for Healthcare significantly vary for several reasons. Quality healthcare for everyone is a global concern. Health equity needs urgent attention not only in the U.S. but worldwide.
Here are six key barriers that should not hinder health equity in the U.S.
1. Socioeconomic Status: The Class
One of the most evident barriers to health equity in the US is an individual’s class. The unfairness of socioeconomic status determines the benefits of healthcare people receive.
For example,
- Lower-income people have more difficulty receiving healthcare due to monetary constraints.
- Low socioeconomic status people have limited access to transportation, proper housing, and healthcare services.
- Moreover, higher healthcare expenses demoralize people from seeking necessary medical care.
Therefore, an individual’s socioeconomic status defines barriers to even basic healthcare services.
Did you know?
Rural counties (58.5%) in the U.S. had lower COVID-19 vaccination coverage with the first primary vaccine series dose than urban counties (75.4%).
2. Racial Discrimination: Race and Ethnicity
An individual’s race and ethnicity is another factor that determines health equity.
- A recent Accenture analysis shows that the medical sector is still far from achieving racial health fairness, but it might eventually happen.
- Moreover, In 2023, the White population surpassed the Black, AI/AN, and Hispanic populations on 70 parameters that assess health and healthcare in America.
Thus, it can be inferred that when compared to their white counterparts, members of racial and ethnic minorities face excessively high rates of illness, disability, and early death.
3. Health Illiteracy
Around 90% of U.S. adults deal with health literacy, emphasizing the need for knowledge and skills.
- To understand health information
- Navigate the healthcare system, and
- Make informed decisions
People with high health literacy can understand medical instructions, prescription drugs, and labels. They can also ask appropriate questions and interact clearly with healthcare providers.
Conversely, people with limited health literacy fail to comprehend health information. This results in missed treatments, misunderstandings and poorer health results.
4. A Lack of Adequate Insurance Coverage
Not all Americans have access to affordable healthcare and do not have the advantages of Medicaid or Medicare. Reduced out-of-pocket costs can be achieved with adequate insurance benefits, such as premiums, co-pays, and deductibles.
According to a report, the uninsured US population in 2024 accounts for approximately 27 million.
Moreover, insufficient coverage to pay medical bills forces individuals to skip necessary care, such as preventive screenings, pediatric visits, dental and vision.
5. Language Barriers
When healthcare providers and patients don’t share a common language, it poses a significant challenge for healthcare systems.
Do you know? 2019 saw nearly 68 million people speaking a language apart from English at home, as per a recent U.S. Census Bureau Report.
It impacts the quality of care, hospital service, and risk of miscommunications or mistranslations.
6. Labour Shortages in Healthcare
The most concerning barrier to health equity is America’s shortage of healthcare providers.
There is expected to be a 46,000–121,900 physician shortage in the US by 2032, with a need for roughly 25,000–65,000 surgical specialists. The staffing shortage is predicted to affect physicians, nurses, technologists and other healthcare professionals.
Moreover, the alarming part is that it also affects patients in “medical deserts,” burns out the medical staff and declines the quality of care.
Overcoming these hurdles is a major priority. Therefore, we have handpicked a few for you. Let’s have a look.
5 Must-Have Technological Changes for Better Healthcare

Health equity is achievable with technical advancements in the healthcare department if the hurdles above are strategically addressed.
Digital technology can help close the equity gap in various ways – from automating difficult-to-navigate medical bureaucracy processes to easing travel barriers to healthcare access.
Let’s examine a few technological developments that could enhance health fairness.
1. Telemedicine
After the COVID-19 pandemic, there has been a sudden increase in telemedicine or virtual healthcare. Telehealth plays a significant role in ensuring that patients receive appropriate medical care.
According to Statista, as of 2023, over 50% of people surveyed in the United States exhibited increased satisfaction with their care due to telemedicine.
Telehealth provides:
- Remote access to healthcare
- Overcomes transportation and travel issues
- Reduces long waiting times and
- Curtails geographical distance
- Convenient availability of healthcare in rural or underdeveloped regions
Example:
Imagine healthcare providers treating patients living in remote areas virtually. The patient consults with a doctor from the comfort of their home. This helps the patient save time and reduces traveling time and distance.
Therefore, telehealth has made online patient screening and engagement a walk in the park. Patients do not have to set foot in a care facility with telemedicine.
2. Mobile Health Apps or mHealth
Apple Health, Teladoc, and Noom are top mobile healthcare apps changing the defination of healthcare availability in America.
mHealth or mobile health apps are revolutionizing and promoting health care globally. Mobile health applications use digital tools and technologies to:
- Monitor health.
- Ease communication with healthcare providers.
- Provide medical history and more.
Mobile health apps give access to health for a diverse population radically and ethically. Every patient can access services, including virtual consultations and medication reminders.
3. Artificial Intelligence and Machine Learning
The U.S. government agencies, such as the CDC (Centers for Disease Control and Prevention), are modernizing healthcare with AI and MI.
AI and machine learning have the power to promote health equity by improving access to healthcare. By leveraging AI and ML, personalized health treatments can be predicted, and biases can be mitigated.
These technological powerhouses can ensure equal access to quality healthcare when integrated with current-day workflows.
Example:
AI and ML can help create a holistic view of health equity. They can also help fill in missing information and data based on race, ethnicity, social discrepancies and more.
Moreover, AI-powered tools can help with the early diagnosis of acute diseases, such as cancer. AI and ML make it easy to provide better and earlier treatment.
4. Remote Patient Monitoring
Remote patient monitoring (RPM) is a technique medical practitioners use to monitor their patients’ health. It is primarily used to treat chronic diseases outside of a traditional clinical setting.
It impacts health equity in a major way, such as:
- Optimizes staff efficiency
- Combats clinical staff shortages
- Fosters patient and healthcare providers’ connectivity
- Bridges the “barrier to access” by equipping care to every individual
- Diminishes expenses and saves time
RPM benefits caregivers, healthcare providers, doctors, patients and the healthcare system as a whole.
5. Digital Health Literacy Tools
Caring for one’s health is more than seeking medical advice or visiting a clinic or hospital. Health is having at least some basic knowledge about health-related factors, such as first aid, CPR, or stopping bleeding.
However, less than 15% of Americans have a good understanding of health information. The benefits of digital health literacy can help increase this percentage.
The perks of digital literacy are:
- Helping patients and caregivers with easy access to information online.
- Better communication with healthcare providers.
- Easy access to health records.
- Better information on chronic health issues, their symptoms and preventive care.
- Overlaps barriers, such as age, ethnicity, and socioeconomic status, lessening the gaps in health equity.
Digital health literacy is still an emerging technology. But, the ability to engage with digital resources is pivotal.
Take a Step Towards Health Equity
Several issues need attention when it comes to health equity. But no matter the problems, digital changes are already bridging the gap between equity in healthcare.
The ultimate solution to health equity is to curtail the barriers that have led people to fall in the cracks. Because, in the end, health equity should benefit every individual who wants to be on the road to better health.
At LeanSummits, you can unleash innovation through healthcare collaborations. Connect with us now to know more.